Osteoporosis – what you must know
By Dr Sandra Cabot
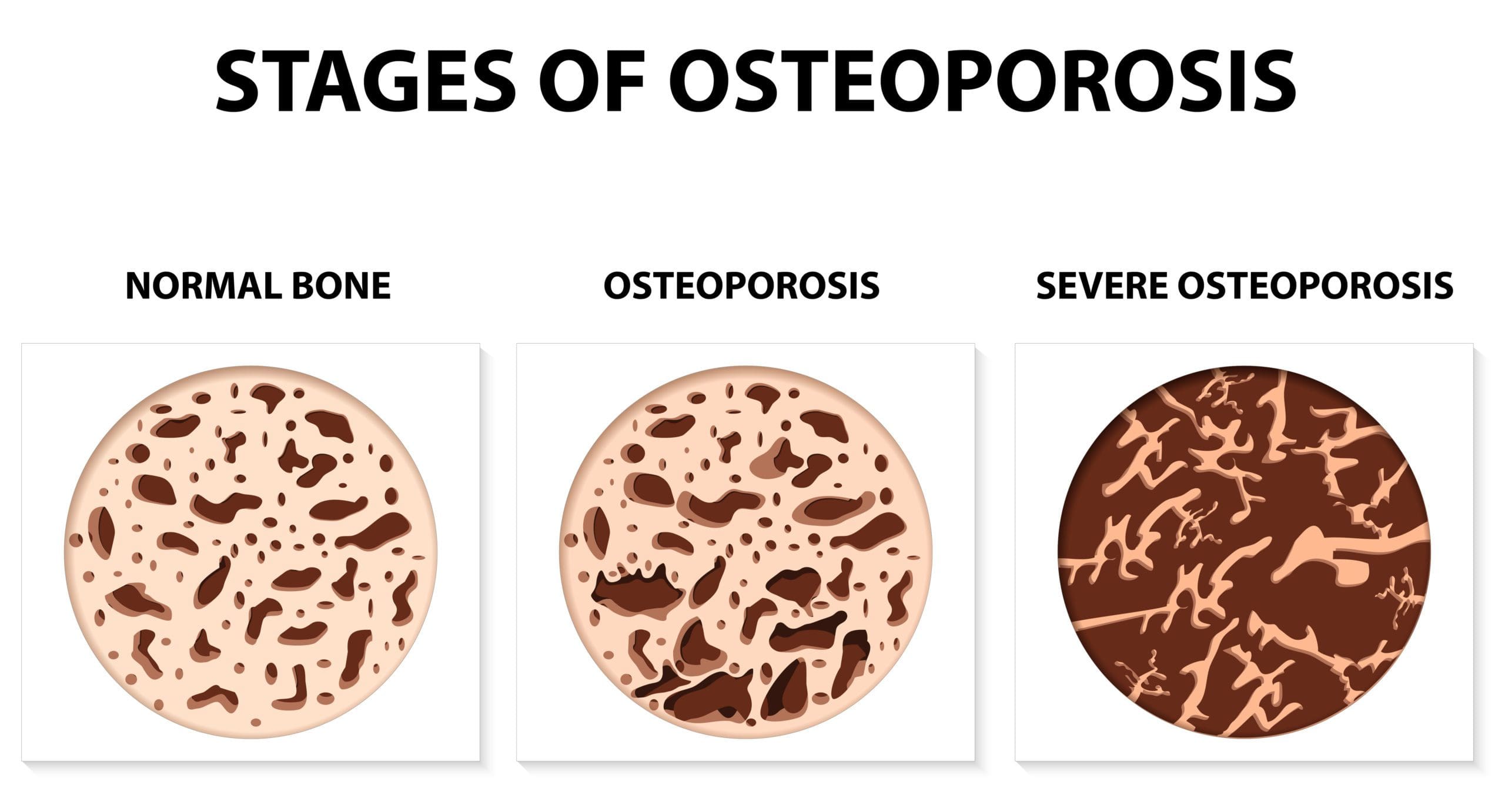
The bone thinning disease of osteoporosis is becoming more common. We can take effective steps to increase and maintain bone strength. You can increase your bone density to safe levels with the right tools.
Osteoporosis is a silent disease in that it is often not diagnosed until there has been a bone fracture and it is then harder to repair the bone damage. It is obviously better to prevent osteoporosis, and this is why it is important to check your bone density with a DEXA test at middle age especially if you have risk factors.
What causes Osteoporosis?
Osteoporosis is NOT just a calcium deficiency. Many factors affect our risk of developing osteoporosis such as:
- Advancing age
- Lack of exercise
- Low levels of vitamin D and vitamin K in your body.
- High levels of parathyroid hormone, which are commonly caused by longstanding unrecognized vitamin D deficiency. The parathyroid hormone levels usually normalize once the vitamin D is supplemented.
- A diet lacking in minerals such as calcium, magnesium, boron, strontium, manganese, zinc, copper and silicon.
- Low intake of vitamin C which weakens the collagen that gives bone its flexibility.
- Low levels of the sex hormones estrogen and testosterone, especially in women with a premature menopause.
- Medications such as long-term corticosteroids, antacid medications (which prevent adequate production of hydrochloric acid in the stomach), excess thyroid medication, and some anticoagulant drugs
- Excess consumption of alcohol and/or cigarette smoking
- Thin build with fine bone structure
- Eating disorders such as anorexia
- Undiagnosed gluten intolerance
- Pancreatic insufficiency with resultant lack of digestive enzymes causing poor absorption of nutrients.
Osteoporosis is not a simple case of not getting enough calcium in the diet and is more related to our modern-day lifestyles. It is also the epidemic of vitamin D deficiency, and if you are low in vitamin D you cannot absorb calcium from your food. You can take a lot of calcium, but if you are vitamin D and/or vitamin K deficient then the calcium is useless!
Factors that cause bone loss
- A mineral deficient diet. Calcium is not the only mineral needed for a strong skeleton. Magnesium, manganese, zinc, silica, boron and copper are essential also. Dairy products such as milk, yogurt and cheese are a source of calcium, but some people are allergic to dairy. Foods high in calcium and other minerals include tinned fish (including the bones), broccoli and bok choy. Refined foods are sadly lacking in all minerals – these include foods made of white flour and white rice. Gluten can reduce the absorption of minerals in many people, especially if they eat large amounts of gluten.
- Lack of physical activity. Sedentary jobs and hobbies promote bone loss as well as muscle loss. Weight bearing exercise helps to strengthen bones, and all exercise helps to maintain balance and flexibility; reducing the tendency of falls that cause fractures.
- A high sugar diet with sodas and diet drinks being especially bad. The high level of sugar and phosphorus in soft drinks is particularly detrimental to bones.
What can you do to prevent osteoporosis?
Vitamin D
Vitamin D3 is made in large amounts from cholesterol in the skin when the skin is exposed to the sun. Vitamin D is actually a steroid hormone and not a vitamin.
In addition to skin manufacture from sunlight, vitamin D can be found in some animal foods. It is also available in supplement form, with the current recommendation being that you take between 400 and 1000 I.U. of vitamin D 3 daily. Many people, especially those who avoid the sun or those living in cold countries, need much more than this. Regardless of how you get it, make sure that you have an adequate amount of vitamin D in your body or your parathyroid hormone will go up and leach precious calcium out of your bones; this can cause kidney stones. It is vitally important to ask your doctor to check your blood level of vitamin D. The correct blood test to measure your vitamin D level is called 25(OH) D, also called 25-hydroxy-vitamin D 3.
Vitamin D can be measured in two different units of measurement and in the USA the units used are ng/mL In Australia and Canada the units of measurement are nmol/L.
The normal ranges of vitamin D for blood tests reported by different laboratories and countries vary significantly and you will be surprised by the large range between lower normal and upper normal – see table below;
Lower Limit Vitamin D Upper Limit Vitamin D
75 nmol/L 200 nmol/L
30 ng/mL 100 ng/mL
You don’t want to be average here; you want to have levels of vitamin D that optimise strong bones. The optimal levels of vitamin D are higher than the average levels. You only want to supplement with natural vitamin D3, which is human vitamin D. The synthetic and inferior vitamin D2 does not work as well as D3.
The synthetic vitamin D used to fortify foods is vitamin D2 (known as ergocalciferol) – it is used to fortify many foods and drinks. In nature, vitamin D2 sources are found in mushrooms, various algae (such as spirulina, chlorella, and blue-green algae) and dark green leafy vegetables, but not in adequate amounts to satisfy human needs.
The other form of vitamin D is D3 (cholecalciferol), which is the kind your body produces as the result of sun exposure, and is also found in some non-vegan foods including egg yolks, butter, and oily fish like mackerel, salmon, sardines, and herring.
I recommend you take enough supplements of vitamin D3 and/or get enough sunshine to keep your serum vitamin D levels around 150 to 200 nmol/L or 70 to 80ng/mL. Excess vitamin D intake can cause elevated blood calcium levels; so, don’t overdose on it – it’s not a case of the more the better. Get your blood level checked every 6 months to find the dose of vitamin D3 that keeps you in the optimal levels.
Vitamin K
Vitamin K is extremely important for those with low bone density as it works in concert with vitamin D to remineralise the bones. Vitamin D is required to absorb calcium from the intestines and to put calcium into the bones. However, the calcium needs to be integrated and spread throughout the bones in the correct places and this is what vitamin K can do. Vitamin K improves the architecture and strength of the whole bone.
What should you eat to beat osteoporosis?


Ensure you consume adequate minerals.
Calcium is not the only mineral needed for a strong skeleton. Magnesium, manganese, zinc, silica, boron, and copper are essential also. Dairy products such as milk, yogurt and cheese are a source of calcium. Not everyone is able to digest dairy products well, or they can aggravate some immune system conditions. A2 milk, raw milk, goat, or sheep dairy products are an option for some people. Non-dairy foods high in calcium and other minerals include tinned fish (including the bones), broccoli, Bok choy and seaweed.


Many people don’t get sufficient vitamin K2.
This vitamin puts calcium into the bones and reduces deposition of calcium in the arteries where you don’t want calcium to build up. The fermented soy food “natto” has the highest vitamin K2 levels of any food; it is an acquired taste and also not available to purchase for many people. Beef and lamb liver are high in vitamin K2. Oily fish, moldy cheese and egg yolks also contain vitamin K2. Leafy green vegetables contain vitamin K1, and good gut bugs can convert it into K2, but people with poor gut health lack these beneficial microbes.
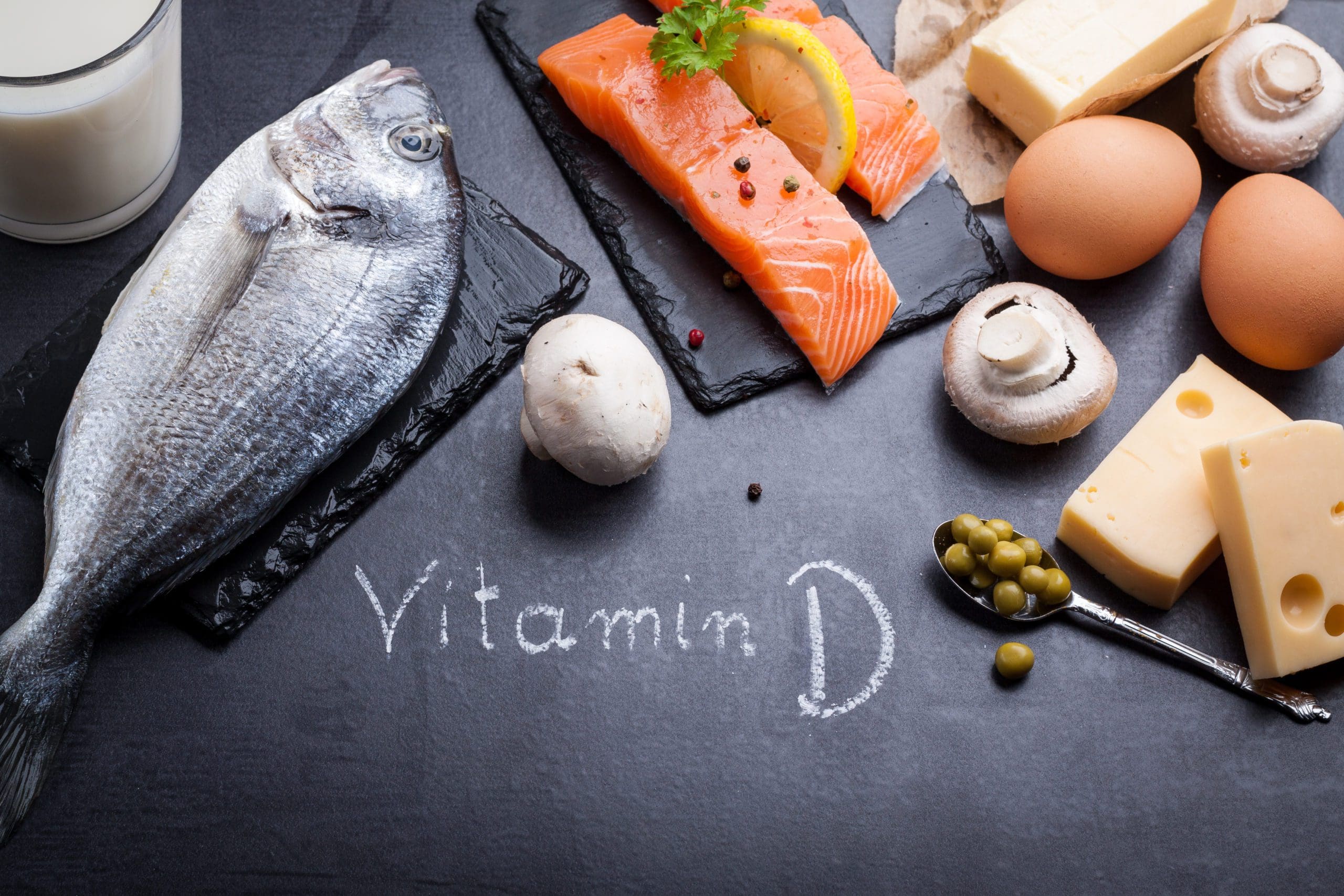
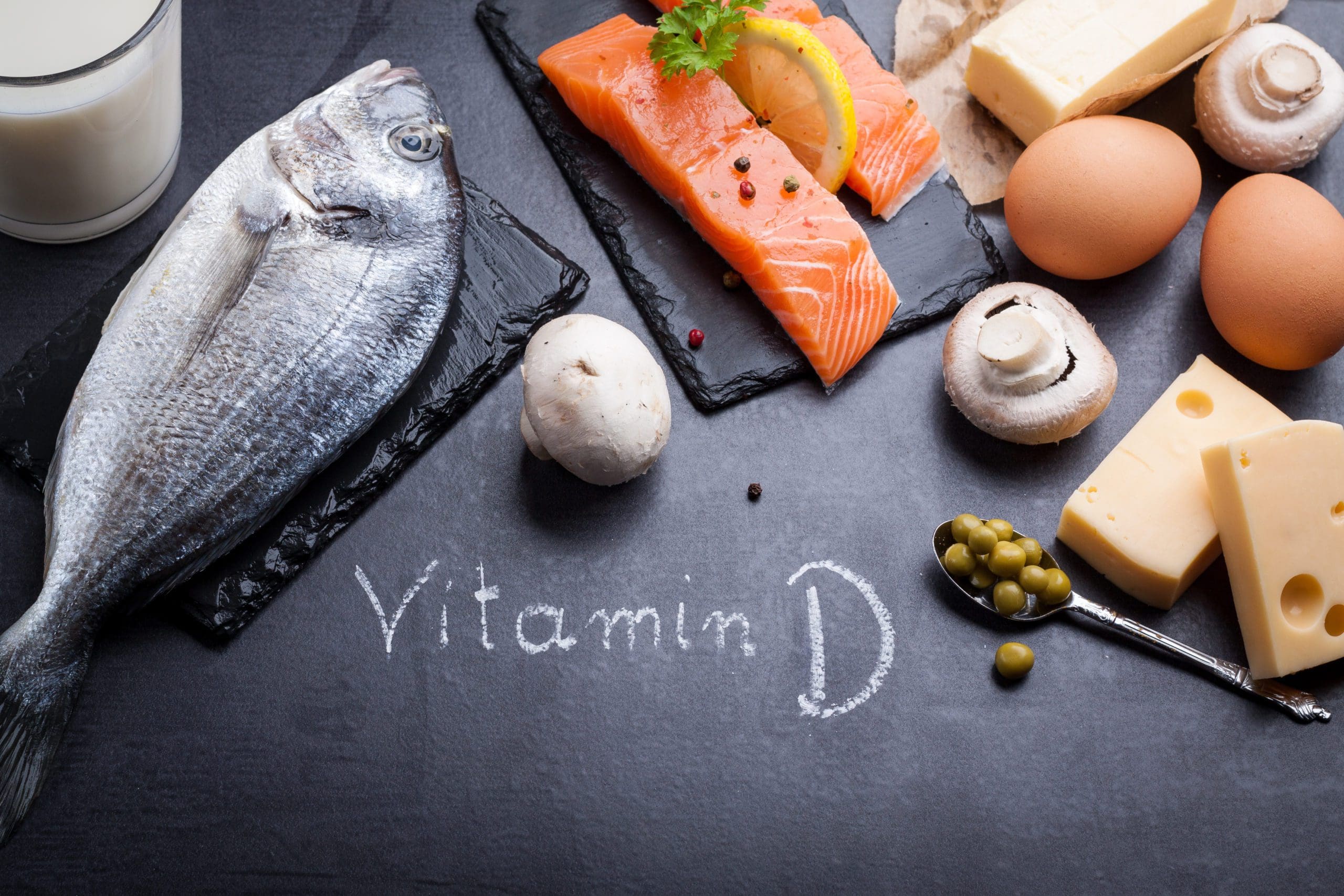
Vitamin D enables calcium absorption.
A few foods contain vitamin D; these include oily fish, eggs yolks, cod liver, full fat dairy products and the fat on meat.


Make sure your body can produce sufficient collagen.
Vitamin C, zinc, biotin, silica and sulphur are required for collagen production. Your bones are made of 70 percent hard collagen, which is a type of protein. Collagen Food Powder contains all these things and can be added to drinks.


Consume adequate protein-rich foods.
Meat, seafood, poultry, eggs and whey protein all help provide your body with the building blocks for all types of protein synthesis, including collagen. Your bones need plenty of good quality protein to be strong.


Magnesium is an essential supplement for strong bones and tendons.
Indeed 80% of the magnesium in your body is found in your bones and for good reason – magnesium is a mineral that gives your bones more density and weight.


Bone Building Supplement
Calcium Complete contains a well absorbed form of calcium known as calcium hydroxyapatite, as well as calcium citrate, plus the other bone essential minerals magnesium, manganese, zinc, silica, boron, and copper. Dose required varies depending on severity of your osteoporosis. You need 1 capsule daily if it is mild (osteopenia) or 2 capsules daily if it is osteoporosis.
Be aware that the cheap form of calcium called calcium carbonate is the most common form of calcium to be advertised. Calcium carbonate is the same form of calcium that is found in chalk and is not well absorbed or utilized by the body.
What can I do if I have osteoporosis?
Talk to your doctor about the use of treatments to prevent bone loss. You may need to see an endocrinologist who specializes in treatment of osteoporosis.
You will need to take the minerals and vitamins mentioned above on a regular basis and must also ensure that your blood vitamin D levels are optimal.
You need a regular exercise program, even if it is only walking 30 minutes a day. With exercise, it’s the more the better, as exercise has been proven to increase bone density.
Talk to your doctor about the use of bio-identical hormones such as testosterone, oestrogen and progesterone, especially if you have had an early menopause, or if your blood levels of testosterone are very low. These hormones can be given in the form of a cream or troches.
Bisphosphonate drugs –
The conventional treatment for osteoporosis is a class of drugs taken by mouth known as Bisphosphonates. Examples are the brands Fosamax and Actonel. Bisphosphonate drugs work by stopping bone turn over – in other words, they stop the breakdown and building of bone. I have never felt comfortable prescribing this class of drugs because Bisphosphonates can have irreversible side effects. These include necrosis (death) of the jawbone, atypical fractures which do not heal well and gut dysfunction. It is generally accepted, but not always adhered to, that Bisphosphonate drugs should only be taken for a maximum of 5 years to avoid such awful side effects.
Denosumab (Prolia) Injections –
Prolia is injected every 6 months. Prolia is effective in stopping bone loss but can have side effects including an increased risk of infections, skin problems (such as rashes, blistering, itching, cracking, dryness, or reddening of the skin) and aches and pains especially in the arms and legs.
The scary thing to me about Denosumab is that if you quit using it suddenly, this may increase your risk for more bone fractures, and they will not heal well. You could be worse off than before you started this drug.
You must tell your doctors that you are receiving denosumab injection, including your dentist. If you are having dental procedures on this drug, you may have an increased chance of having a severe problem with your jaw. To put it bluntly your jawbone may die!
Long term use of Prolia may increase your risk of developing fractures of the thigh bone which may present as a dull or aching pain in the thigh, groin, or hips.
Many people cannot tolerate the prescription drugs commonly used to prevent and treat osteoporosis. They may be nervous about potential side effects which can be severe.
Strontium for stronger bones –
Strontium is a naturally occurring mineral present in the soils, food and water. The availability of strontium from food, like many other minerals, depends upon the content of strontium in the soils of the regions where the produce is grown; thus, food is an unreliable source of strontium.
Do not confuse strontium with toxic radioactive Strontium-90, as they have entirely different effects in the body.
Trace amounts of strontium are found in the human skeleton and strontium is naturally absorbed at the bone matrix crystal surface. The effects of strontium on bone metabolism have been researched since the 1950’s and trials have shown that strontium improves bone metabolism by promoting new bone formation and decreasing bone breakdown; this promotes normalised bone density.
How do you know if you have low bone density?
The gold standard test to measure how dense (strong) your skeletal bones are is called a DEXA test and is widely available. DEXA stands for Dual Energy X-ray Absorptiometry. A DEXA test can measure bone density in the spine, hip, forearm, and the total body. It is one of the most common methods to determine bone density as it is fast, painless and highly accurate. The amount of radiation used in DEXA scans is very low and similar to the amount of radiation used in common x-rays. Pitfalls in DXA are common, and errors can be categorised as patient positioning, data analysis, artefacts, and/or demographics. When DXA studies are performed incorrectly, it can lead to major mistakes in diagnosis and management. Measurement error must be considered when evaluating serial assessments. Initial screening for osteoporosis should be performed according to National Osteoporosis Foundation (NOF) recommendations. The optimal interval for repeating DEXA scans is uncertain, but because changes in bone density over short intervals are often smaller than the measurement error of most DEXA scanners, frequent testing (e.g., < 2 years) is unnecessary in most patients. Even in high-risk patients receiving drug therapy for osteoporosis, DEXA changes do not always correlate with probability of fracture. Therefore, DEXA should only be repeated if the result will influence clinical management or if rapid changes in bone density are expected. Recent evidence also suggests that healthy women 67 years and older with normal bone mass may not need additional DEXA testing for up to 10 years provided osteoporosis risk factors do not significantly change.
The majority of these procedures are quick and pain-free. Dual energy x-ray absorptiometry (DEXA), which uses a special x-ray scanning machine to measure bone density, is the most popular technique as it is fast and highly accurate. Another name for bone density testing is bone mass measurement.
If you have any questions on osteoporosis you can phone our friendly advisors on 0246554666
References
Wright, J.V., Fight – Even Prevent – Osteoporosis with the hidden secrets of this bone-building miracle mineral. (Reprint from Nutrition and Healing. Tahoma Clinic, 2008)
DeHart, S.S. (July 7, 2008). Strontium and Osteoporosis: A treatment not offered to American Women
Dean, W. (May 2004) Strontium breakthrough against Osteoporosis







Leave A Comment