Covid raises the risk of autoimmune disease
By naturopath Margaret Jasinska
COVID infection increases the risk of developing an autoimmune disease in genetically susceptible people.
Research conducted in South Korea looked at 354,527 people diagnosed with COVID-19 via a polymerase chain reaction (PCR) test from October 8, 2020 to December 31, 2021. The researchers compared the COVID-19 group to 6,134,940 healthy people who didn’t get COVID-19 to assess the risk for autoimmune and autoinflammatory connective tissue diseases. They found the risk of alopecia areata, alopecia totalis, antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis, Crohn’s disease, and sarcoidosis were higher in people who had a COVID infection.
People who experienced such a severe COVID-19 infection that they were admitted to the ICU were at greater risk for several autoimmune conditions, including alopecia totalis, psoriasis, vitiligo, and vasculitis.
It has been known for a long time that infections can be a trigger for autoimmune disease. This doesn’t happen in everyone; it tends to happen in people with a genetic susceptibility to autoimmune disease. People with autoimmune disease in their family. The infection can be like the straw that breaks the camel’s back, causing an autoimmune disease in at-risk individuals. Long COVID is a condition a high percentage of people have developed. It is a long lasting inflammatory state with chronic fatigue-type symptoms. I believe in some people this is a pre-autoimmune condition. The grey zone before an actual autoimmune disease can be diagnosed.
The Epstein Barr virus that causes glandular fever is one of the most well known viral triggers of autoimmunity.
This virus is in the herpes family of viruses and is an extremely common infection that just about everyone has suffered from at some point in their life. It’s quite a sinister virus though; it is capable of triggering 33 different autoimmune diseases. Obviously not everyone who has had glandular fever goes on to develop 33 autoimmune diseases, let alone one. This virus is simply one of the known triggers.
The Epstein Barr virus is most closely linked with the development of multiple sclerosis, systemic lupus erythematosus, rheumatoid arthritis and Sjogren’s syndrome. Research has shown that some people with systemic lupus erythematosus have an elevated Epstein Barr viral load in their bloodstream. It may be more than 15 times greater than in healthy individuals. This means that some people are unable to clear the virus from their bloodstream because they have a weak immune system. The chronic stimulation of the immune system by the virus may go on for many years, and eventually lead to the development of an autoimmune disease.

Streptococcal infections are very common.
Strep throat is sometimes responsible for a sore throat, fever and enlarged lymph glands in the neck. The most common cause of a sore throat is a viral infection, while streptococcus is a type of bacteria. It is thought to be responsible for approximately 37 percent of cases of sore throat in children and only 5 to 15 percent in adults.
A small percentage of people who have had a strep infection go on to develop rheumatic fever, which is an autoimmune disease caused by antibody cross reactivity. The white blood cells had been producing antibodies against the strep bacteria, but for some reason the immune cells become confused and start making antibodies against the heart, skin, joints or brain. The surface molecules on the strep bacteria are so similar to some molecules of the human body, that a small percentage of people who get a strep infection go on to develop an autoimmune disease. Rheumatic fever can cause arthritis, myocarditis (inflammation of the heart), a skin rash and Sydenham chorea (a brain disease that causes involuntary movements of the face and arms). Strep infections are also capable of triggering autoimmune kidney disease (glomerulonephritis), PANDAS (Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections) and Tourette syndrome.
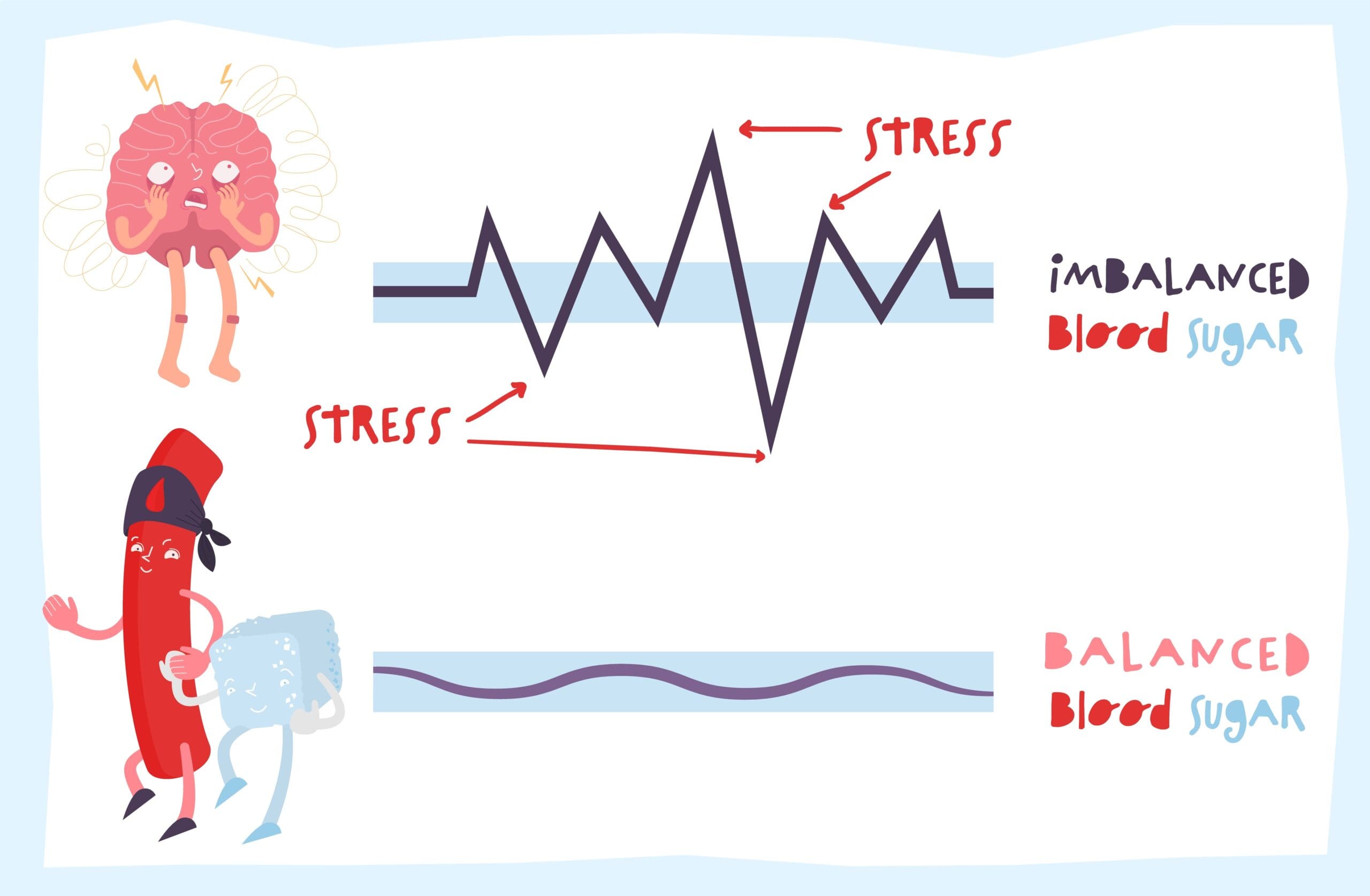
If you don’t recover quickly from an infection, the infection has more time to have destructive effects on your health.
If you are stressed, not sleeping enough, not eating well and have nutrient deficiencies, this is more likely to be you. Almost all of my patients are found to have nutrient deficiencies when we test them.
Fortunately there is a lot that can be done to improve the health of a person with autoimmune disease, and many people are able to recover fully. For more information see our book Healing Autoimmune Disease: A plan to help your immune system and reduce inflammation.





Leave A Comment